Varicose veins in the lower extremities are a problem that precedes more than 60% of the world’s population. The term "varicose vein" from the Latin word "varix" is interpreted as "expansion. "Therefore, the definition of the pathological condition - the dilation of the lumen of the veins of the lower extremities and pelvic organs, which significantly impairs blood flow in the blood vessels and, accordingly, worsens the general condition of the patient. In the following, we examine the causes of varicose veins, the possible complications of the disease, and the main ways to treat the pathology.
Causes and risk factors: Everyone is prone to this
Important:if the varicose veins reach young people under the age of 25, here the gender distribution is 50: 50. That is, both boys and girls are equally ill. In adulthood, varicose veins are more common in women due to pregnancy and age-related significant hormonal changes.
If the varicose veins are considered from the inside, anatomically, the dilation of the venous lumen occurs due to a failure of the venous valves that regulate blood flow. Malfunctioning valves do not close completely with every heartbeat. As a result, blood jerking from the heart moves to the lower limbs due to gravitational force.
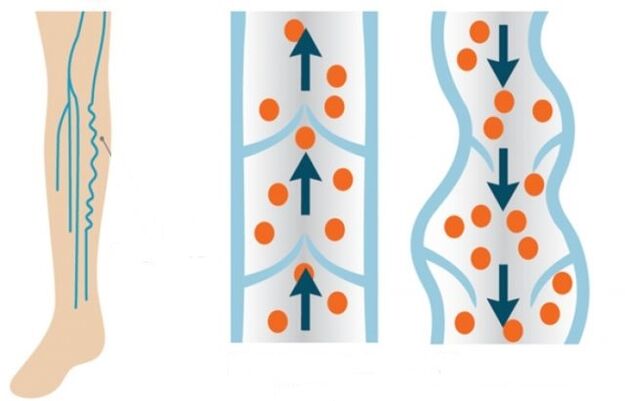
Normally, the valves should close and allow blood to flow in part into the legs. But unfortunately, blood flow enters the legs more intensely and moves less intensely in the opposite direction due to the same malfunction of the valve system. The veins in the legs that overflow with blood lose their elasticity over time and lengthen.
The main predisposing factors for the development of vascular disease are:
- genetic component (the disease can spread through a female or male line within the family);
- overweight;
- postponed pregnancies;
- passive lifestyle;
- excessive physical activity;
- smoking and alcohol consumption;
- hormonal disorders.
Male problems
If we consider the causes of varicose veins, depending on the sex of the patient, they differ somewhat in men and women. More specifically, members of different sexes are all prone to certain habits that may sooner or later provoke pathology of the vessels of the lower extremities. So for men, the risk factors are:
- strength training by lifting dumbbells from squats;
- overweight and obesity;
- an unbalanced diet that causes frequent constipation;
- pathological processes of the kidneys (tumors of different etiologies);
- groin hernia;
- sedentary work;
- smoking and alcohol consumption.
Important:men are characterized not only by the development of varicose veins of the lower extremities but also of the spermatozoa. This pathology is called varicocele. Such a condition is inherited, that is, it is purely genetic in nature, and even enhanced preventive measures do not prevent it. Only 2-4% of men suffer from varicocele. The cause of the pathology is the asymmetric anatomical location and structure of the male genitals.
Due to the fact that men suffer from false meanness or do not have time to see a specialist at the very beginning of the disease, varicose veins are more difficult for them than for women.
Women’s varicose veins have their own laws
Varicose veins are "better known" in women than in men. More than 80% of women suffer from vascular pathology of the legs. In addition, the risk group includes the nicer sex who prefer this lifestyle or experience the following conditions:
- wearing tight, high-heeled shoes;
- sitting or standing work;
- hereditary predisposition;
- changes in hormonal levels during pregnancy or in autoimmune diseases;
- wearing too tight underwear, jeans;
- smoking;
- low percentage of fruits and vegetables in the diet (constant diet and starvation);
- love of tanning (frequent visits to the solarium or direct sunlight);
- sharp weight gain;
- low mobility.
Pregnancy is where the "dog is buried"
Even if manifestations of varicose veins, the causes and treatment of which need only be determined and prescribed by the phlebologist, are not initially observed in a woman, they become apparent in 30% of cases during pregnancy. Here, the main pitfall lies in the growing fetus, and with it in the uterus, which intensely compresses the pelvic organs. As a result, the blood circulation in the lower body is significantly damaged. It is difficult for blood to return from the legs upwards. This effect on the deep veins of the legs leads to the fact that the vessels are actively stretched in both width and length.
In addition to the growth of the uterus and the pressure on the vessels of the pelvic organs, the varicose veins of pregnant women also develop as a result of the following factors:
- Increased blood clotting. Thus, nature secures a woman against great blood loss during childbirth. Thicker blood is harder to move through the blood vessels.
- An increase in the level of the hormone progesterone, which leads to relaxation of the muscles and blood vessels in the uterus, so it can grow freely and without tone as the fetus grows. But at the same time, the walls of the remaining pots also relax. The veins are less flexible, and thick blood stretches the walls already weakened by progesterone even more.
- An increase in blood pressure to improve the oxygen supply to the fetus. As a result, the body tries to quickly draw thick blood through the relaxed blood vessels. The volume of the legs increases as a result.
- Pregnant woman low mobility with abdominal growth. This leads to stagnation of blood in the legs and pelvic organs.
Complications of varicose veins
If varicose veins are not treated and paid attention to them, over time, the patient may develop very serious complications that may even require full surgical intervention. In the worst case, the patient may undergo amputation of the patient's limb. The most common and dangerous complications of varicose veins are considered below.
Chronic venous insufficiency
With the development of such a complication, active failure of the venous valves occurs. In addition, the pathological process is divided into four stages:
- Zero. After a difficult day, the patient feels mild swelling and rare pain in the legs.
- First. The venous network of dilated blood vessels becomes visible on the surface of the skin.
- Second. Swollen veins, blood clots and nodules are clearly visible. There are redness, itching, sores at the site of inflamed veins.
- Third. Trophic ulcers develop with inflamed veins in the legs.
Important:signs of chronic venous insufficiency include itchy legs, pain, burning sensation in a prolonged sitting position, swelling, night cramps.
The superficial veins are thrombophlebitis
In this case, the patient is prone to blood clots. Blood clots actively block the lumen of the veins, making it difficult for blood to flow. In most cases, blood clots and blood clots are localized in the vessels of the lower third of the thigh or upper third of the leg. Symptoms of venous thrombophlebitis include:
- redness of the skin of the legs at the site of clot formation;
- pain in the legs;
- palpation - induration in the veins.
Important:in case of thrombophlebitis, compression stockings should be worn. The compression formula should be selected by a specialist, an angiosurgeon or a phlebologist.
Trophic ulcer
This complication manifests itself in the later stages of venous insufficiency. First, the patient shows increased vascular permeability. A whitish seal is formed on the skin surface, which has a lacquer-like surface. An ulcer forms underneath. At the slightest damage to the inflamed area, the ulcer opens and the exudate begins to separate. A leaking wound can become secondarily infected, leading to purulent inflammatory processes.
Important:in this condition, complete wound healing is required first, and only then is complete surgery performed to remove the affected vessels.
Pulmonary embolism
It is an equally dangerous complication when the thrombus detaches from the inflamed vein and moves toward the pulmonary artery. This artery is directly involved in organizing blood flow in a small circle, affecting the right ventricle of the heart. If the diameter of the detached thrombus is smaller than the lumen of the artery, the clot moves toward the branches of the pulmonary artery, causing pulmonary edema or infarction. In this case, the patient will experience significant chest pain. A wet cough mixed with blood, a rise in body temperature and weakness also appear. If the diameter of the clot is equal to the diameter of the pulmonary artery lumen, immediate occlusion and death will occur for the patient.
Clot detachment can be caused by the following conditions:
- performing surgical procedures;
- oncology;
- heart failure;
- long bed rest.
Conservative and surgical treatment
Varicose veins can be treated in both conservative and operative ways, depending on the stage of the pathology and the condition of the patient. In case of conservative treatment, the administration of phlebotonic drugs is recommended. On the outside, horse chestnut-based gels and venotonic ointments are used. It should be understood that conservative treatment only works in the initial stages of varicose veins.
Additional measures for conservative treatment of varicose veins include physical activity (walking) and wearing compression stockings.
Minimally invasive and surgical treatment methods
If the process of varicose veins and venous insufficiency has gone far, they will resort to minimally invasive or full-fledged surgical intervention to improve the patient’s condition. Minimally invasive intervention methods include:
- Sclerotherapy. In this case, a special sclerosing drug is injected into the lumen of the patient’s varicose veins using a thin insulin needle. The injected substance causes inflammation first and then sclerosis of the affected vein. The lumen of the diseased vessel simply grows. The technique has more of a cosmetic effect, but does not solve the problem (cause) of the pathology itself. Relapses are possible after sclerotherapy. A contraindication to such an intervention is pregnancy, lactation, and intolerance to the components of the drug.
- Stripping. With this method, the patient's vein is removed with the thinnest probe. The peculiarity of the surgical procedure is that only the sick part of the vessel can be removed, leaving its healthy parts. The operation is performed with two endoscopic punctures located on either side of the site of the inflamed vessel. That is, scars and scars after such an intervention will not be visible.
- Microflebectomy. Removal of a diseased vein is also done through several small incisions in the skin.
- Laser coagulation. Laser exposure to the lumen of a diseased vessel. As a result, the lumen of the vein is completely overgrown.
Complete surgery (abdominal surgery) is called phlebectomy. With this method, the surgeon makes a complete incision in the skin of the foot in order to remove the entire superficial vein. The signs of such an operation are as follows:
- large amount of varicose veins;
- large cavity (lumen) of diseased vessels (more than 10 mm);
- thrombophlebitis;
- the presence of a large varicose vein;
- development of trophic ulcers in the patient;
- lack of effectiveness of minimally invasive surgery.
Traditional treatment methods
In the early stages of the pathology, you can also use folk methods of treating varicose veins. In particular, in combination with medication, you can use the following folk remedies:
- The tomatoes are green. Thin slices of vegetables are placed in the area of inflamed veins and fixed with a bandage. You should change such applications every 2-3 hours. The cure lasts until the condition clearly improves.
- Potato. A bandage soaked in freshly squeezed potato juice is placed on the legs. Cover the top with foil. Such applications are most likely to be performed at night until the patient's condition improves.
- Apple vinegar. Preferably homemade. Dilute the vinegar with water (1 glass of water and 2-3 tablespoons of vinegar). The dressing is moistened in solution and placed in the area of the diseased veins. The bandage is fixed at night. You can easily lubricate your feet at night with this solution. It has been shown to take in vinegar water and inside. Add 1 tablespoon of apple cider vinegar and a teaspoon of honey to a glass of water so as not to burn the esophagus with vinegar (the walls of the esophagus are very sensitive to acids). Drink the mixture in the morning on an empty stomach. The process of vinegar treatment is 30 days.
- Horse chestnuts. The flowers of the plant in an amount of 50 gr. pour 0, 5 liters of alcohol and insist for two weeks in a dark place, shaking the mixture regularly. The finished product is filtered through a mesh and we drink three times a day, one tablespoon each. The mixture is washed with water. The cure is 7 days. Then a 14-day break and again a seven-day course. Treatment according to this schedule is performed until the end of the infusion. The therapeutic regimen can then be reconstituted and repeated.
- Burdock. In this case, fresh leaves of the plant are used to eliminate the disease. At night, the sore legs are smeared with Vishnevsky ointment and wrapped on top of burdock. Everyone is bandaged and put on compression stockings. The bandage is worn for three days, then removed and everything is washed away. During the summer it can be treated this way while fresh burdock grows.
Important:such treatment is contraindicated in patients with high gastric acid content.

conclusions
It is worth recognizing that varicose veins are in most cases irreversible pathologies. That’s why it’s so important to take care of the health of your feet. Especially if you have a genetic predisposition to varicose veins. It is enough to give up bad habits, balance your daily diet, walk more and drink enough clean water daily. When the slightest signs of varicose veins appear, it is advisable to contact a competent phlebologist immediately to prevent complications of the disease. Remember that your health and the internal condition of your feet are entirely up to you. And modern medicine and the hands of a specialist can work wonders.























